Healthcare Financial Services IG Edition 1 - Local Development build (v1.0.0) built by the FHIR (HL7® FHIR® Standard) Build Tools. See the Directory of published versions
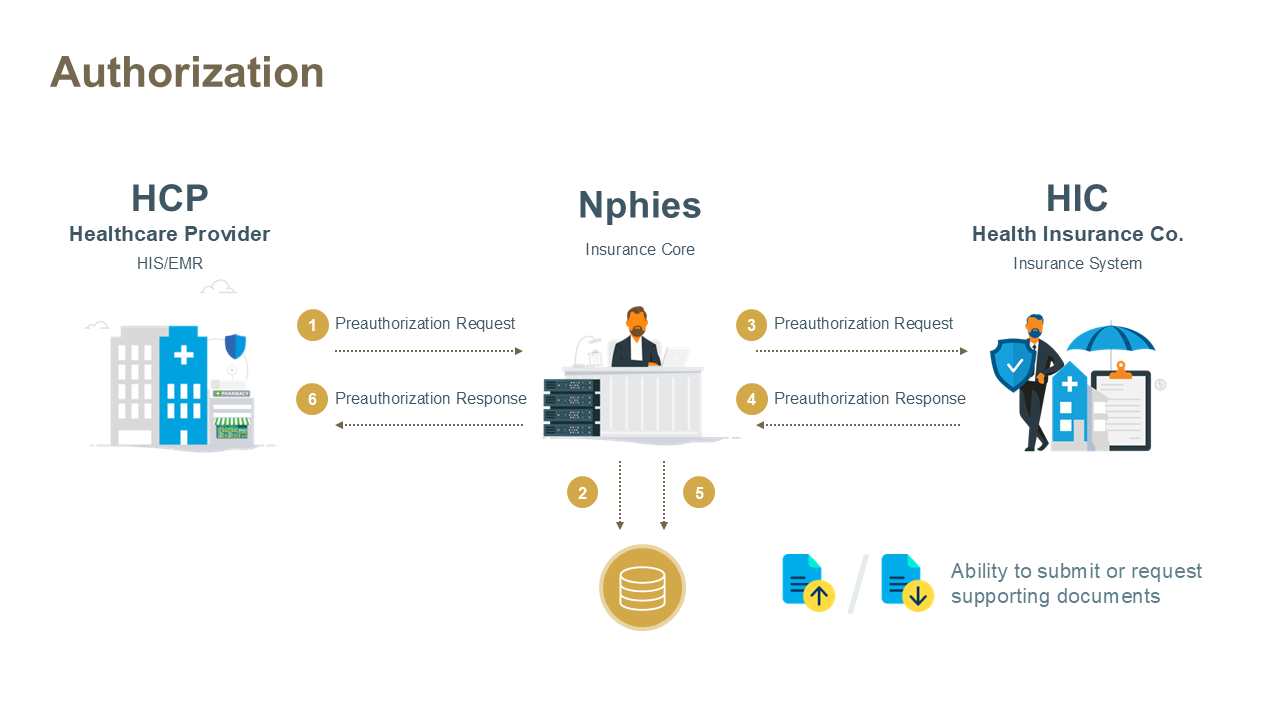
This use case enables healthcare providers (HCPs) to obtain approval from the Health Insurance Company (HIC) before delivering healthcare services to beneficiaries. The Prior Authorization (PA) process ensures that the requested services or treatments meet payer criteria for coverage and reimbursement. Providers submit an authorization request to nphies, which validates and routes the request to the respective insurer or Third-Party Administrator (TPA). The insurer then adjudicates the request and responds with errors, approval, denial, or a request for additional information. If approved, then the insurer provides a reference to include on Claims for the approved services.
Prior Authorizations may be processed as real-time transactions or non-real-time transactions, depending on the insurer's adjudication capabilities:
The key resources for the message are provided below and all require nphies-profiled resources as provided in the Artifacts. Note: the MessageHeader resource must be the first .entry in the bundle and any other resources may follow in any order.
The key resources for the message are provided below and all require nphies-profiled resources as provided in the Artifacts. Note: the MessageHeader resource must be the first .entry in the bundle and any other resources may follow in any order.
There are five types of prior authorization handled within the nphies system:
Each type of authorization follows a similar request-response pattern but may have specific extensions or required data elements.
Authorizations are managed by an insurer as a dynamic file of planned, and sometimes performed, products and services. The sections below detail how providers manipulate the effective contents of each dynamic authorization file.
Providing Eligibility: Providers SHALL include information about the Eligibility Check if one was performed prior to the authorization or claim. This information is provided through the Eligibility Response extension if the check was performed online via the Eligibility use case or if eligibility checking was done manually, for example on a portal or over the phone, via the Eligibility Offline Reference extension and the Eligibility Offline Date extension.
SupportingInfo – Days Supply: Required for outpatient medications using the 'days-supply' category code (see the days-supply slice on supportingInfo). Not required for inpatient items.
The first authorization request for an intended suite of goods and services to treat a patient results, assuming at least one of the line items is accepted, in the creation of the dynamic authorization file and the return of an authorization reference in the ClaimResponse.preAuthRef element of the authorization response.
The provider may change the list of requested services by submitting a new authorization request containing the previously supplied .preAuthRef in the authorization request. The new authorization request must contain ALL of the goods and services to be performed including both those which has been previously approved and those which have been completed. For completed line items which the insurer had previously approved the provider SHALL provide the .servicedDate, which may be today or in the past, and insurers SHALL return a response indicating the item is approved - insurers SHALL NOT reject or otherwise alter the approval previously given for the line item. Providers and insurers SHALL also preserve the .item.sequence values across requests and responses to ease alignment and understanding.
Examples: The examples below assume the original authorization request included four service lines (sequence=1,2,3,4), all of which were approved,
A provider may need to cancel an authorization if, for example: the treatment plan changes; the patient no longer wishes to proceed with the authorized services; or, the provider or practitioner is no longer available to provide the services on a timely basis. The provider SHALL issue a cancel-request with the identifier to the previously approved authorization in the Task.focus element. Providers SHALL NOT cancel authorizations where the ClaimResponse.preAuthPeriod has expired as this authorization is effectively cancelled.
Use Case A provider is unable to provide some services to the patient and therefore needs to request the transfer of services to another provider by sending a prior authorization for the transfer to the patient’s insurer. Referral Prior Authorization handling on nphies Follow the below steps to process Patient Referral Prior Authorization on nphies:
Example of the transfer extension
“extension”: [
{ “url”: “http://nphies.sa/fhir/ksa/nphies-fs/StructureDefinition/extension-transfer”,
“valueBoolean”: true
}
]
| Example | Description |
|---|---|
| Example #1 Request | Standard prior authorization request for DayCase. |
| Example #1 Response | Insurer approves the requested service with an authorization reference number. |
| Extension | Description |
|---|---|
| Adjudication Outcome | A code indicating the outcome of the adjudication such as rejected, partially approved/paid or approved/paid as submitted. |
| Adjudication Reissue Reason | The reason the adjudicator has reissued an authorization or claim response. |
| EligibilityResponse | CoverageEligibilityResponse ID from the original eligibility request-response exchange. |
| EligibilityOffLineReference | A reference value from the payer from a manual (offline) eligibility request. |
| EligibilityOffLineDate | Date when the offline check was done. |
| Encounter | An extension to referring to the encounter. |
| Maternity | To confirm if this item will be counted under the maternity benefit. |
| Newborn | Flag to identify that this authorization is for a newborn. |
| Package | A package billing code or bundle code used to group products and services to a particular health condition. |
| PatientShare | The patient share amount. |
| PayerShare | The expected payer share amount (to be paid). |
| Tax | The amount of Tax (VAT) levied on the line item. |
| Transfer | Flag to indicate an authorization to transfer services to another provider. |
| TransferAuthorizationNumber | Transfer approval authorization number. |
| TransferAuthorizationPeriod | Transfer approval authorization period. |
| TransferAuthorizationProvider | Transferred to provider. |
If nphies or the Insurer, or TPA on behalf of an insurer, detect errors in the request message such that the request cannot be processed then the response message will contain an OperationOutcome resource rather than a business-level response message.
Similarly, if the nphies system times-out on passing the request message to the Insurer/TPA or times-out on receiving a valid response from the Insurer/TPA or receives an invalid response from the Insurer/TPA then the nphies system will return a message with an OperationOutcome to indicate the nature of the error. If the response message is issued by nphies rather than the Insurer/TPA then a Bundle.meta.tag will be included to document that.
Like all other response messages the provider receives from nphies, if there are other messages queued at nphies which have not been delivered to the provider then this will be reflected in the presence of a MessageHeader.meta.tag. These queued messages may be retrieved by the provider at their convenience, see Polling for guidance on Polling, Pended Message retrieval.