Healthcare Financial Services IG Edition 1 - Local Development build (v1.0.0) built by the FHIR (HL7® FHIR® Standard) Build Tools. See the Directory of published versions
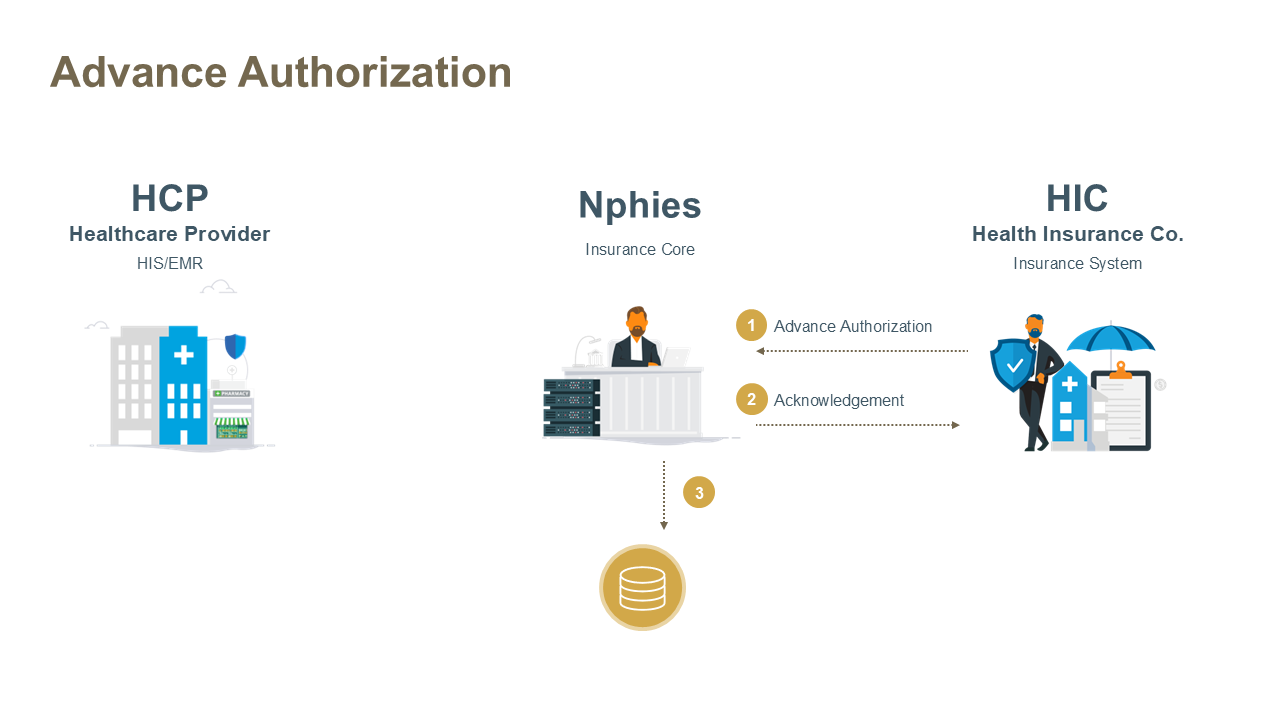
This use case enables Health Insurance Companies (HICs) to initiate and send an Advanced Authorization (Approval) to the Healthcare Provider (HCP) without receiving a prior authorization request. This transaction supports specific scenarios where the HIC proactively grants approval for services or treatments. The advanced authorization is sent to the nphies platform, which routes it to the appropriate HCP. The HCP polls for and retrieves the Advanced Authorization when available.
Advanced Authorization is typically used in scenarios where services are pre-approved outside the standard request-response flow, such as bundled care programs, chronic disease management and refills, or payer-driven initiatives requiring proactive authorization.
HCPs will use the Poll Request to fetch the Advanced Authorizations (APA) available in nphies.
The key resources for the message are provided below and all require nphies-profiled resources as provided in the Artifacts. Note: the MessageHeader resource must be the first .entry in the bundle and any other resources may follow in any order.
| Example | Description |
|---|---|
| Typical Advanced Authorization | HIC sends the Advanced Authorization to HCP in order to provide required services to the patient. HCP receives Prior Authorization on treatment for a patient without submitting prior authorization. |
| Modify/add additional item on a received APA | If the HCP intends to modify/add additional items on a received Advanced Authorization from an HIC, the HCP should
send a new prior authorization request including all the approval items (existing and additions/modifications) and including the preAuthRef received in the APA. The previous Advanced Authorization is considered overridden by the new Authorization Request. |
| Requesting for modification or extension |
|
This use case permits both the HCP and HIC to cancel the Advanced Authorization.
| Example | Description |
|---|---|
| Example #1 | An advanced authorization to a hospital for oral services. |
| Example #1 Acknowledgement | An Acknowledgement response indicating message was received and understood or was with errors. |
| Extension | Description |
|---|---|
| Adjudication Outcome | A code indicating the outcome of the adjudication such as rejected, partially approved/paid or approved/paid as submitted. |
| Adjudication Reissue Reason | The reason the adjudicator has issued an advanced authorization. |
| Advanced Authorization Reason | The reason the adjudicator has reissued an authorization or claim response. |
| Diagnosis | Information about diagnoses relevant to the advanced preauthorized items. |
| Maternity | To confirm if this item will be counted under the maternity benefit. |
| Newborn | Flag to identify that this authorization is for a newborn. |
| Package | A package billing code or bundle code used to group products and services to a particular health condition. |
| Prescription | Prescription to support the dispensing of pharmacy, device or vision products. |
| Referrer Provider | The referring provider. |
| Service Provider | The party who will provide the services. |
| Supporting Information | Additional information codes regarding exceptions, special considerations, the condition, situation, prior or concurrent issues. |
| TransferAuthorizationNumber | Transfer approval authorization number. |
| TransferAuthorizationPeriod | Transfer approval authorization period. |
| TransferAuthorizationProvider | Transferred to provider. |
If nphies detects errors in the request message such that the request cannot be processed then the response message will contain an OperationOutcome resource rather than a business-level Status Response resource. Otherwise if nphies detects errors within the request it will return a Status Response with errors (Task.output.type = 'error') and an extension indicating where the error occurred.
Like all other response messages the provider receives from nphies, if there are other messages queued at nphies which have not been delivered to the provider then this will be reflected in the presence of a MessageHeader.meta.tag.