Healthcare Financial Services IG Edition 1 - Local Development build (v1.0.0) built by the FHIR (HL7® FHIR® Standard) Build Tools. See the Directory of published versions
This use case enables the HCPs to verify the beneficiary’s insurance coverage, to check whether the insurance is currently active (in-force) and whether the plan will pay for healthcare services provided at the given facility. Additionally, the provider can request the benefit details associated with the plan. Note: if the provider does not know the patient insurance (coverage) details then the provider may use the HIDP-API to obtain a list of the patient's insurance so they can then send the eligibility checks to those insurers.
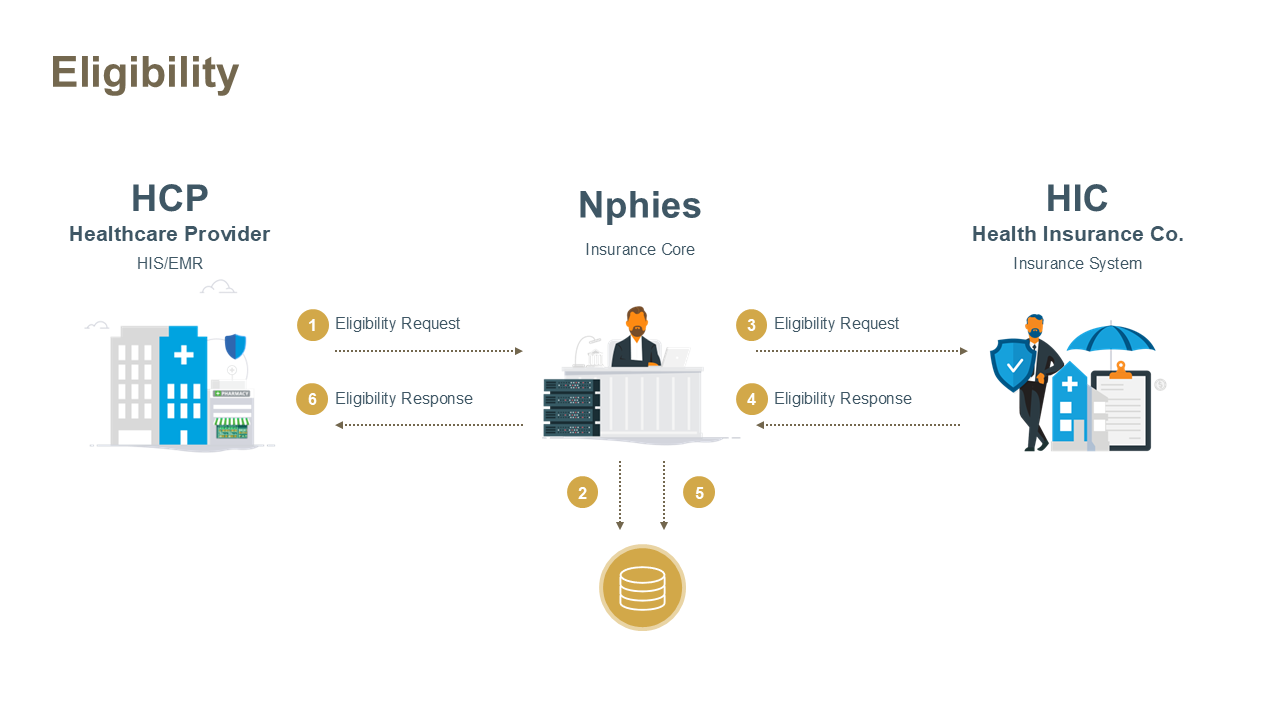
This is a REAL TIME use case. In the event that nphies is not able to successfully deliver the Eligibility Request Message to the HIC within one minute then nphies will generate a response message, with a bundle.meta.tag to identify that the message has been issued by nphies, see Meta Tag: nphies-generated.
The key resources for the message are provided below and all require nphies-profiled resources as provided in the Artifacts. Note: the MessageHeader resource must be the first .entry in the bundle and any other resources may follow in any order.
On eligibility requests for a newborn, add the Newborn extension if required. On eligibility requests for a transfer of care, add the Transfer extension.
The key resources for the message are provided below and all require nphies-profiled resources as provided in the Artifacts. Note: the MessageHeader resource must be the first .entry in the bundle and any other resources may follow in any order.
A new element (Site Eligibility) has been added to the eligibility response, through the inclusion of the Site Eligibility extension, to inform the provider whether the patient is eligible to have their services covered by the insurance. A value of "eligible" indicates that the patient is eligible, and other codes indicate that the patient is not eligible.
The below Site Eligibility extension example is provided if the CoverageEligibilityResponse.outcome is "complete."
{
“extension”: {
“url”: “http://nphies.sa/fhir/ksa/nphies-fs/StructureDefinition/extension-siteEligibility”,
“valueCodeableConcept”: {
“Coding”: [{
“system”: “http://nphies.sa/Terminology/CodeSystem/siteEligibility”,
“code”: “eligible”
}]
}
}
}
The actions which the provider is expecting the insurer to perform are indicated by the codes submitted via the *.purpose element. The codes and expected insurer actions are shown below:
| Code | Description | Required Elements |
|---|---|---|
| benefit | The plan benefits and optionally benefits consumed for the listed, or discovered if specified, coverages are requested. | Option 1: Patient Identifier + Coverage Option 2: Patient Identifier + “Discovery” as eligibilityrequest-purpose |
| discovery | The insurer is requested to report on any coverages which they are aware of, in addition to any specified, which would be active on the specified .servicedDate. | Patient identifier |
| validation | A check that the specified coverages are in-force at the requested .servicedDate. | Option 1: Patient Identifier + Coverage Option 2: Patient Identifier + “Discovery” as CoverageEligibilityrequest.purpose |
In the event that the provider is unable to deliver the Eligibility Request to nphies or nphies is unable to deliver the request to the insurer or TPA then the provider is directed to use other means such as an insurer portal or support desk to check patient eligibility. For manual eligibility checks, the provider should record the date and the eligibility reference provided by the insurer or TPA for submission on subsequent authorizations and claims.
| Example | Description |
|---|---|
| Example #1 Request | Eligibility Request asking for benefits and validation. |
| Example #1 Response | Eligibility Response responding to request asking for benefits and validation. |
| Extension | Description |
|---|---|
| Newborn | Flag to identify that this request is for a newborn and therefore the coverage supplied will be for the Mother of the patient not the patient. |
| Site Eligibility | Code to indicate whether the patient is eligible to have their services paid by their insurance and if not eligible the code indicates why the services are not covered. |
| Transfer | Flag to indicate a request to transfer services to another provider. |
If nphies or the Insurer, or TPA on behalf of an insurer, detect errors in the request message such that the request cannot be processed then the response message will contain an OperationOutcome resource rather than a business-level Eligibility Response resource.
Similarly, if the nphies system times-out on passing the request message to the Insurer/TPA or times-out on receiving a valid response from the Insurer/TPA or receives an invalid response from the Insurer/TPA then the nphies system will return a message with an OperationOutcome to indicate the nature of the error. If the response message is issued by nphies rather than the Insurer/TPA then a Bundle.meta.tag will be included to document that.
Like all other response messages the provider receives from nphies, if there are other messages queued at nphies which have not been delivered to the provider then this will be reflected in the presence of a MessageHeader.meta.tag. These queued messages may be retrieved by the provider at their convenience, see Polling for guidance on Polling, Pended Message retrieval.