Healthcare Financial Services IG Edition 1 - Local Development build (v1.0.0) built by the FHIR (HL7® FHIR® Standard) Build Tools. See the Directory of published versions
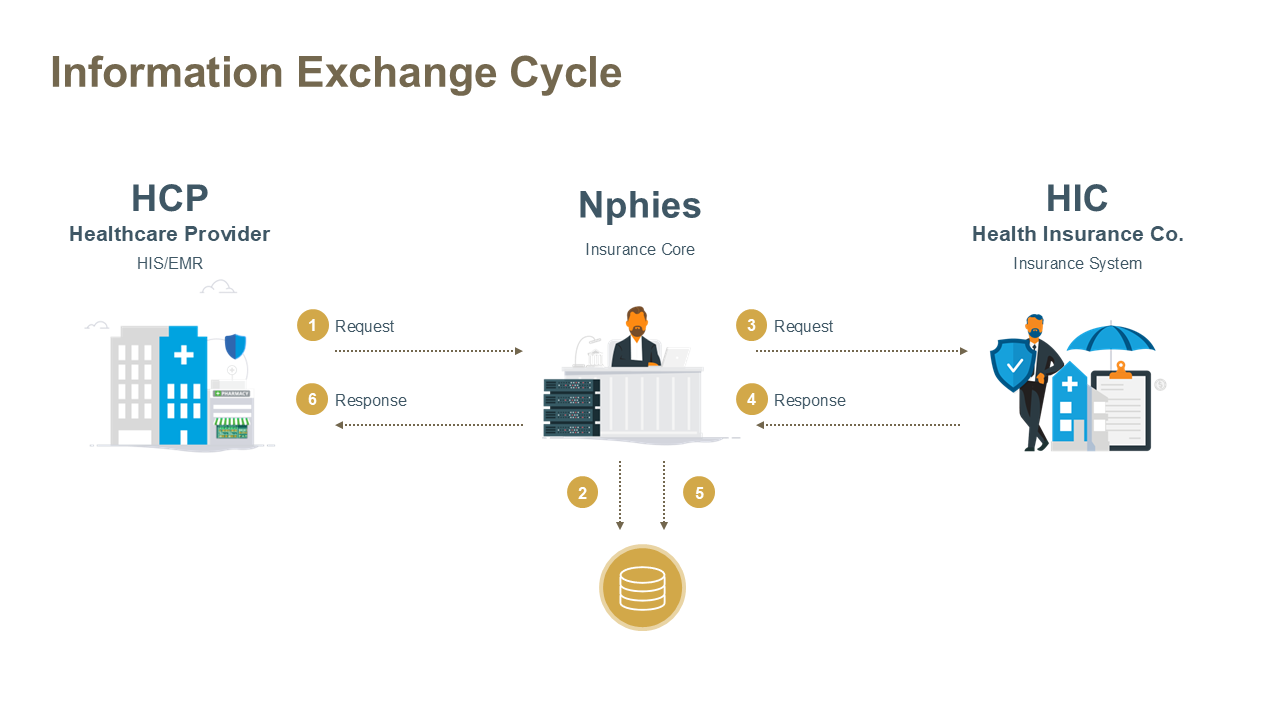
nphies is a centralized network and processing system, which will connect all stakeholders to efficiently and effectively manage and monitor the standards-based information exchanges between providers (Hospitals, Clinics, Pharmacies, Optical shops [collectively referred to as HCPs]) and payers (Health Insurance Companies (HICs) and TPAs) for the benefit of all stakeholders including the beneficiary.
| Actor | Description |
|---|---|
| HCP | HCP role represents the HCP staff/ backend systems that will be interacting with nphies to conduct the health insurance business processes (Eligibility, Prior Authorization, Claims, and Payment Management Services) through nphies. |
| HIC | HIC role represents the HIC staff/ backend systems that will be interacting with nphies to conduct the health insurance business processes (Eligibility, Prior Authorization, Claims, and Payment Management Services) through nphies. |
| TPA | TPA role represents the TPA staff/ backend systems that will be interacting with nphies to conduct the health insurance business processes (Eligibility, Prior Authorization, Claims, and Payment Management Services) through nphies. TPAs act on behalf of HICs. |
| nphies | nphies role represents the electronic platform that will be acting as the integration hub between all stakeholders involved in the health insurance business in the Kingdom. |
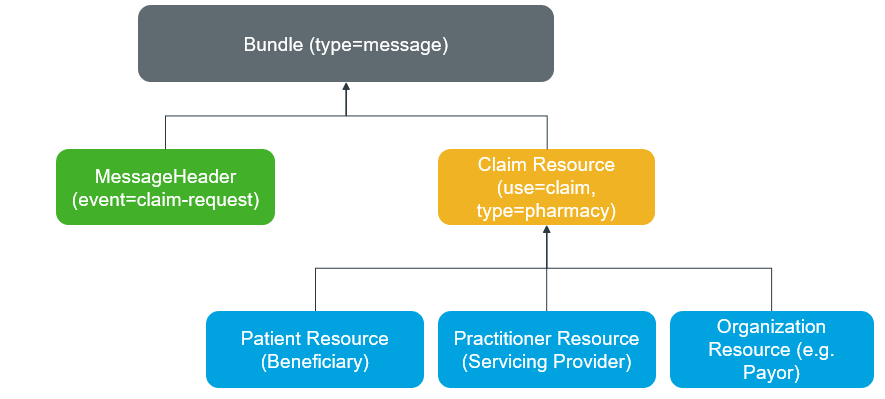
The basic content model in FHIR is the resource, a topic-specific collection of data elements, e.g., a Patient, Organization, Encounter, or Claim, which contains the data elements to support that topic and refers to other Resources to provide the information elements for that topic. Complex information exchanges such as all the information to document an Encounter is modeled as an Encounter resource which provides certain information on the encounter and refers to the appropriate Patient, Practitioner and Observation, etc. resources.
HL7 FHIR supports a variety of exchange patterns including point-to-point FHIR RESTful (CRUD) exchange of individual resources; FHIR Operations with defined input and output parameters; exchanges of groups (Bundles) of resources to Message, Document, and other operational endpoints; and the exchange of single resources or resource Bundles over any non-FHIR specified transports such as FTP, SMTP (email), WSI web services, etc.
The business exchanges needed to support eClaim in Saudi have a few defining characteristics which guide the selection of content packaging and content exchange in FHIR:
This leads to one general packaging guidance, that all needed resources to support the intended information exchange should be included in the same package except where references are made to commonly accessible repositories such as may exist for images, labs, and medications. Given the design of the nphies ecosystem and financial information exchange requirements, nphies is implementing FHIR Messaging as a combination of synchronous and asynchronous exchange of FHIR Message Bundles each containing one, or more when permitted, suite of HL7 FHIR Resources which constitute a coherent information exchange such as an eligibility request or claim.
The message bundle is exchanged via the $process-message operation endpoint of the gateway.
All the mentioned use cases in this guide SHALL refer to one endpoint operation e.g. https://hsb.nphies.sa/$process-message or such $process-message endpoint provided by testing and production sites.
Note: conformance testing environments, and general testing environments and their related pseudo-payer conformance applications are set up and designed for technical development and testing purposes. Therefore, implementers SHALL refrain from transacting or sharing any real patient or confidential information through them. Ensure that all Person Identifying Information (PII) and Personal Health Information (PHI) data is masked and dummy information is utilized when executing any testing scenario.
The process message operation accepts a message, processes it according to the definition of the event in the message header, and returns one or more types of response messages.
Process Message Structure will have in-parameters (Input) and out-parameters (Output).
|
|
Information exchanges will be satisfied with a combination of real-time synchronous request-response and asynchronous FHIR messaging of information models such as eligibility request and response, claim status check and response, and polling for outstanding responses and return of the response.
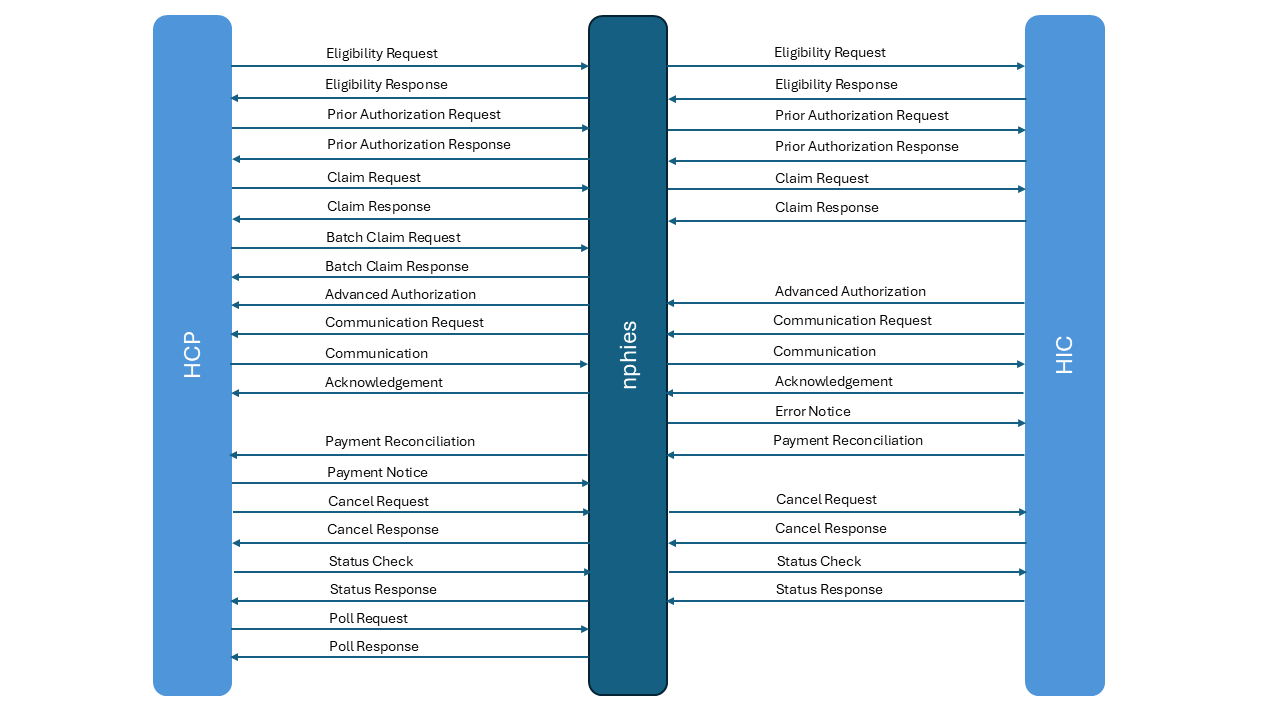
The diagram below depicts the typical exchange through the central gateway for exchanges with payers and assumes loose coupling of the gateway front-end (provider side) and back-end (payer side) processes. See the Message Exchange section for greater detail on the steps and actions expected at each step.
Real time business processing means that the completed business response to a request is provided as the response to the request, for example the adjudicated response to a claim or authorization request, and deferred business processing means that the completed business response will be provided at a later time and the response to the request will be to acknowledge receipt of the request or provide a validation level response only. While all point-to-point exchanges are real time and the overall exchange design supports real-time end-to-end exchange of business-level message, some use cases are defined to be real time only, others are deferred only and other use cases can support both real time and deferred business processing. A notice indicates that there is no direct business response expected, although an acknowledgement from the immediate receiver is expected, as the notice is the business response and/or a statement of request where the business response, if any, is expected later or out of band. The Use Cases addressed by this guide and the type of business processing is shown below:
| Group | Use Case | Business Processing Expectation |
|---|---|---|
| Eligibility | Eligibility Checking | Real time |
| Authorization | Prior Authorization | Real-time and Deferred |
| Advanced Authorization | Notice | |
| Claims | Claim Submission | Real Time and Deferred |
| Claim Batch | Deferred | |
| Payment | Payment Notification | Notice |
| Payment Reconciliation | Notice | |
| Communication | Information Submission | Real Time and Deferred |
| Information Request | Notice | |
| Supporting | Cancellation | Real Time |
| Error Notice | Real Time | |
| Polling | Real Time | |
| Status Check | Real Time |
The hierarchical representation of the sample structure of FHIR Bundle Resource is shown as below:
The list below of codes will be used as the .eventCoding in the MessageHeader of the respective transactions. Selecting the link on the event codes below leads to the event message structure in one of the Use Cases where the message is used.
| Message Event Code | Description |
|---|---|
| acknowledgement | Message with just a MessageHeader, and optional referenced OperationOutcome if there are errors, to acknowledge the receipt of a message. |
| advanced-authorization | A response without existing request for prior authorization of products and services. |
| batch-request | A request for adjudication of a batch of claims for products and services. |
| batch-response | A response to a request for adjudication of a batch of claims for products and services. |
| cancel-request | A request to cancel the processing, whether complete or not, of a prior submission such as a claim. |
| cancel-response | A response to request to cancel the processing, were complete or not, of a prior submission such as a claim. |
| claim-request | A request for adjudication of a claim for products and services. |
| claim-response | A response to a request for adjudication of a claim for products and services. |
| communication | A provision of supporting information in response to a request or to support a prior submission. |
| communication-request | A request for supporting information for a previously submitted request. |
| eligibility-request | A message requesting the identified patient’s insurance, determination if the insurance is in force, and potentially requesting the table of benefits or other insurance details. |
| eligibility-response | A message responding to the Eligibility Request with errors or insurance details. |
| error-notice | A message sent from nphies to HIC to indicate a prior response from the HIC contained errors. This message identifies the prior message and the type of error |
| payment-notice | A notice providing the current status of a payment. |
| payment-reconciliation | A report of a payment and the allocation of the payment to the respective claims being settled. |
| poll-request | A request for the next 'n' undelivered messages from the queue of undelivered messages for the requester. |
| poll-response | A message responding to a poll-request containing up to 'n' requested undelivered messages. |
| priorauth-request | A request for prior authorization of products and services. |
| priorauth-response | A response to a request for prior authorization of products and services. |
| status-check | A request to check on the processing status of a prior submission. |
| status-response | A response to a request to check on the processing status of a prior submission. |
The message event codes, presented below, are from the KSA Message Events CodeSystem.
| Transaction | Focal Resource | Message Event Code |
|---|---|---|
| Acknowledgement | N/A | acknowledgement |
| Advanced Authorization | Claim | advanced-authorization |
| Batch Claim Request | Bundle | batch-request |
| Batch Claim Response | Bundle | batch-response |
| Cancel Request | Task | cancel-request |
| Cancel Response | Task | cancel-response |
| Claim Request | Claim | claim-request |
| Claim Response | ClaimResponse | claim-response |
| Information Submission | Communication | communication |
| Information Request | CommunicationRequest | communication-request |
| Eligibility Request | CoverageEligibilityRequest | eligibility-request |
| Eligibility Response | CoverageEligibilityResponse | eligibility-response |
| Error Notice | OperationOutcome | error-notice |
| Payment Notice | Payment | payment-notice |
| Payment Reconciliation | PaymentReconciliation | payment-reconciliation |
| Poll Request | Task | poll-request |
| Poll Response | Task | poll-response |
| Prior Authorization Request | Claim | priorauth-request |
| Prior Authorization Response | ClaimResponse | priorauth-response |
| Status Request | Task | status-check |
| Status Response | Task | status-response |
The table below lists the transactions which use the Task resource to accomplish a processing behavior and the Task.code value which indicates the type of activity requested.
| Activity | Code | Description |
|---|---|---|
| Cancel Request | cancel or nullify | To request that the activity associated with a prior message be cancelled regardless of whether it has begun or completed processing. If nullify is specified, then the original message may be retained for audit purposes but shall not be given out or displayed. Task.focus.identifier = a business identifier (e.g., Claim.identifier) of the main resource of the message to be cancelled. Optional Task.input.type = ‘nullify’ and Task.input.valueBoolean = ‘true’. |
| Cancel Response | cancel or nullify | HCP to respond on a received APA from HIC that the associated activities will be cancelled regardless of whether it has begun or completed processing. Task.focus.identifier = a business identifier (e.g., ClaimResponse.identifier) of the main resource of the message to be cancelled. |
| Poll Request | poll | To request the next ‘n’ messages be returned from the nphies queue. Typically, these are messages which have not previously been delivered. See Polling. |
| Poll Response | poll | To provide the the next ‘n’ messages be returned from the nphies queue based on the .input selection parameters with each message returned as a separate element in the .output array. |
| Status Check | status | To request the processing status of a message, for example for the adjudication of a claim. Task.focus.identifier = a business identifier (e.g., Claim.identifier) of the main resource of the message to be checked. |
| Status Response | status | Returns the processing status of the specified message. |
Extensions are the FHIR technique for including custom yet standardized additional data elements into a data structure, or even a data element, to provide additional information not otherwise defined in the base FHIR data standard. The guide will use some extensions already defined in the FHIR R4 specification and also defines some new extensions just for the purpose of this guide.
The MessageHeader resource is required on all request and response messages, however there are differences in a few of the elements used depending upon whether it is a request or a response, and whether the message it generated by nphies as shown in the table below.
| Element | Used By | Request or Response |
|---|---|---|
| extension.originalRequest | nphies only | Error Notice Request |
| extension.originalResponse | nphies only | Error Notice Request |
| response.identifier | Any | Response |
| response.code | Any | Response |
| response.details | Any | Response |
Tags, or coded values, MAY be inserted in the MessageHeader.meta.tag array of response messages sent from nphies to Providers to provide processing advise:
Although a polling check is a relatively light transaction, the load can become considerable if many providers are checking at a high frequency. While a formal subscription-publication model could be instituted the methods proposed below are lighter, require less maintenance and have been found to provide the same or similar results depending upon the types of providers:
{
"resource":{
"resourceType": "MessageHeader",
"id": 123,
"meta": {
"lastUpdated": "2020-12-13",
"profile": [...],
"tag": [{
"system": "http://nphies.sa/terminology/CodeSystem/meta-tags",
"code": "queued-messages"
}]
}
...
}
While the response to a request sent to an intended recipient will normally come from that recipient, periodically nphies will be required to generate an interim response on their behalf. In those circumstances the response will have a 'nphies-generated' tag in the MessageHeader. For example:
{
"resource":{
"resourceType": "MessageHeader",
"id": 123,
"meta": {
"lastUpdated": "2025-01-13",
"profile": [...],
"tag": [{
"system": "http://nphies.sa/terminology/CodeSystem/meta-tags",
"code": "nphies-generated"
}]
}
...
}