Healthcare Financial Services IG Edition 1 - Local Development build (v1.0.0) built by the FHIR (HL7® FHIR® Standard) Build Tools. See the Directory of published versions
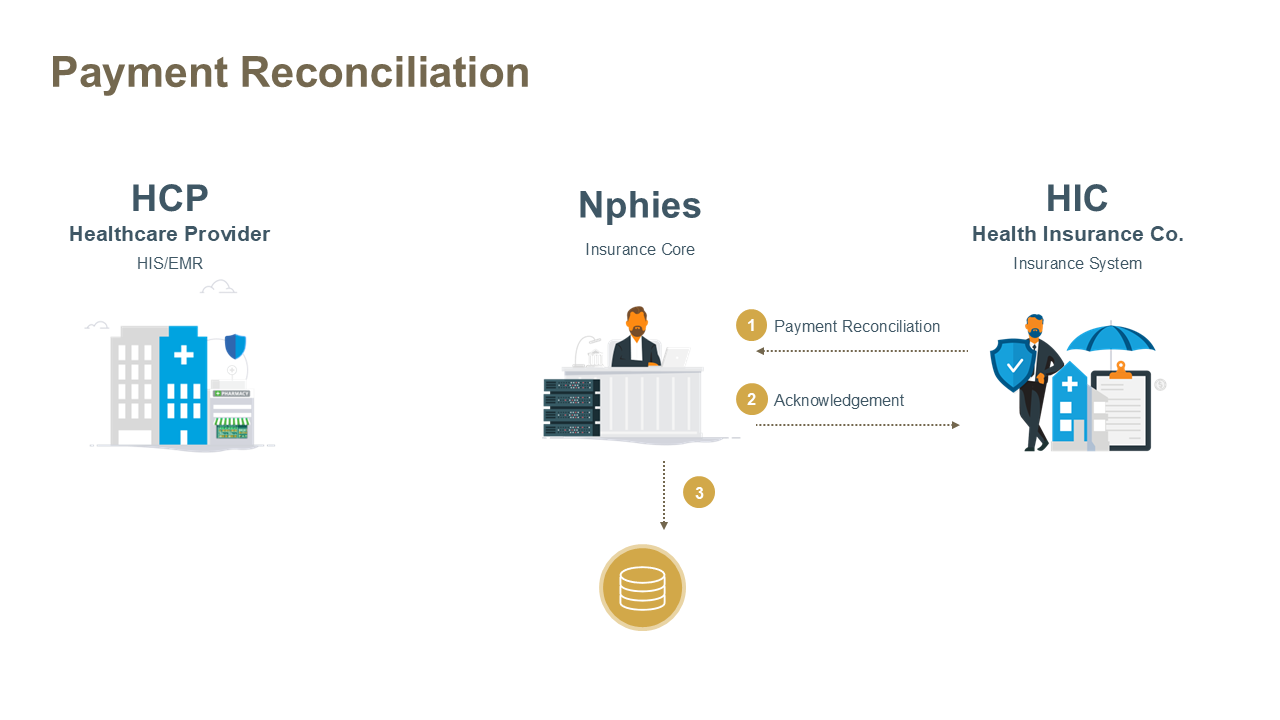
This use case enables Health Insurance Companies (HICs) to notify Healthcare Providers (HCPs) that payment for one or more adjudicated claims has been issued. The HIC provides detailed allocation information regarding the payment using a PaymentReconciliation resource. This transaction ensures transparency and traceability of claim settlements between payers and providers.
The key resources for the message are provided below and all require nphies-profiled resources as provided in the Artifacts. Note: the MessageHeader resource must be the first .entry in the bundle and any other resources may follow in any order.
The PaymentReconciliation is used by HIC to advise HCP how the HIC allocates funds within a payment from the insurer to the provider, regarding:
Payments may also include specification of adjusting factors such as nphies fees, a service fee levied for the nphies service, or early payment fees, a service fee levied by the insurer or payment issued in a 'shorter than normal' payment cycle.
See also: Information Guides.
| Example | Description |
|---|---|
| Example #1 | Full message for Payment Reconciliation. |
| Example #1 Acknowledgement | An Acknowledgement response indicating message was received and understood or was with errors. |
| Extension | Description |
|---|---|
| Component Early Fee | The charge for early settlement of the payment. |
| Component nphies Fee | The charge for nphies services. |
| Component Payment | The amount of the payment. |
If nphies detects errors in the request message such that the request cannot be processed then the response message will contain an OperationOutcome resource rather than a business-level Status Response resource. Otherwise if nphies detects errors within the request it will return a Status Response with errors (Task.output.type = 'error') and an extension indicating where the error occurred.
Like all other response messages the provider receives from nphies, if there are other messages queued at nphies which have not been delivered to the provider then this will be reflected in the presence of a MessageHeader.meta.tag.